What type of facet joint problem are you suffering from? Are you sure that the diagnosis of a facet joint issue correctly explains your pain? This is a question not often considered by many patients, but it should be, since a great number of facet joint pain syndromes are mistakenly diagnosed each year.
Facet joint pain is unlike many other forms of back pain in that is it rarely severe and is basically self-limiting in most profiles. Furthermore, the symptoms of most facet joint conditions are usually very easy to correlate to the diagnosis and should match exactly. When the symptoms do not correlate, misdiagnosis is typically the reason why.
This essay provides guidance for newly diagnosed and long suffering patients with facet joint pain. We will examine what the clinical expectations are for facet joint symptomology and then you can contrast these facts against your own suffering in order to reduce your chances of being misdiagnosed.
Typical Facet Joint Problems
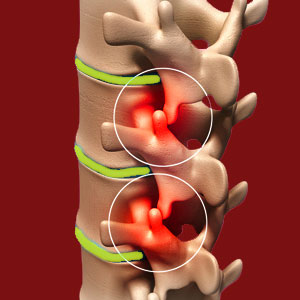
The most common facet joint problem is facet joint syndrome. This is a general name for localized pain in the joint due to a breakdown of the protective mechanisms that allow the joint to function perfectly and subsequent symptomology due to mechanical issues or nerve irritation. Facet syndrome conditions are structurally identical to people with normal facet joint degeneration in virtually all cases. This is one reason why they are misdiagnosed so often. In essence, facet deterioration is universal and people who have pain often have identical degrees of degeneration to people who do not. In fact, many completely asymptomatic people have far worse structural breakdown of the facet joint tissues!
Neurological compression or irritation within the joint will affect small nerves that serve the local tissues. Pain might be acute, but will not be disabling or widespread. Mechanical dysfunction might make the joint painful to mobilize or reduce the effective range of motion in the affected joint. Stiffness and discomfort are common complaints.
In cases of very severe degeneration or traumatic injury, the facet joints can become unstable locally, regionally or throughout the spine. This is a much more serious condition that can facilitate great suffering and more significant spinal issues.
Although not technically a problem of the facet joints, osteophyte growth around the facet joints can reduce the effective space of the foraminal openings and possibly contribute to a compressive neuropathy.
We see many patients with obvious muscular pain in widespread areas being labeled with a diagnosis of facet syndrome, simply because movement intensifies their pain and might produce hot spots of symptoms over the spine. This is criminal negligence!
Diagnosis of Facet Joint Problems
Facet joint pain is difficult to accurately diagnose, since as mentioned earlier, the structural conditions involved are impossible to differentiate from normal spinal degeneration in most cases. In some cases, there exists evidence of obvious pathology, while in others functional examination will raise the suspicion of facet syndrome due to specific areas of painful motion, stiffness or limited ROM. There is no single accurate test for facet syndrome and diagnoses are made subjectively based on an accumulation of evidence.
One of the biggest problems we see when it comes to “confirming” a facet joint diagnosis is the use of anesthetic injections into the joint. If the patient feels better, then the diagnosis is facet syndrome is typically made, despite the truth that the substance can spread regionally and soothe pain from many possible sources. While this type of facet joint injection is the gold standard for diagnostic accuracy, it remains far from perfect and we have spoken out against its reliability for many years already. We have simply seen too many patients who underwent the injections, were labeled with the facet syndrome diagnosis and later turned out to be obviously misdiagnosed. We know because we helped them to find a cure after their treatments and surgeries for facet joint pain failed miserably. In none of these cases did we facilitate cures by continuing to treat these coincidental facet joint scapegoats.
Misdiagnosis of Facet Joint Problems
There is no way to be certain that a facet joint diagnosis is correct barring successful treatment. If pain continues despite treatment, then the chances of misdiagnosis increase dramatically. After all, it is logical that in this age of tightly regulated medical science, the efficacy of indicated treatment exists. Therefore if treatment fails, it is most often due to targeting the wrong condition… We observe this occurrence very often when facet joint surgery fails to produce satisfying postoperative outcomes despite the procedure being judged to be a smashing success from a technical point of view.
If you have been suffering chronic or recurring pain blamed on facet joint pathology, yet treatment has failed you time and time again, then it is obvious to reconsider the validity of the diagnosis, instead of continuing to treat a condition that is not likely to be the actual origin of your symptoms. Failure to understand this basic truth will sentence patients to much unnecessary suffering. It is certainly not a bad idea to seek out multiple diagnostic opinions, especially from different types of care providers with objective and enlightened views of pain.